Qing Zhang, PhD is an Associate Professor, Department of Pathology & Laboratory Medicine and Pharmacology at UNC Lineberger Comprehensive Cancer Center. He and Xianming Tan, PhD are the recipients of KCCure’s 2018 Innovation Award.
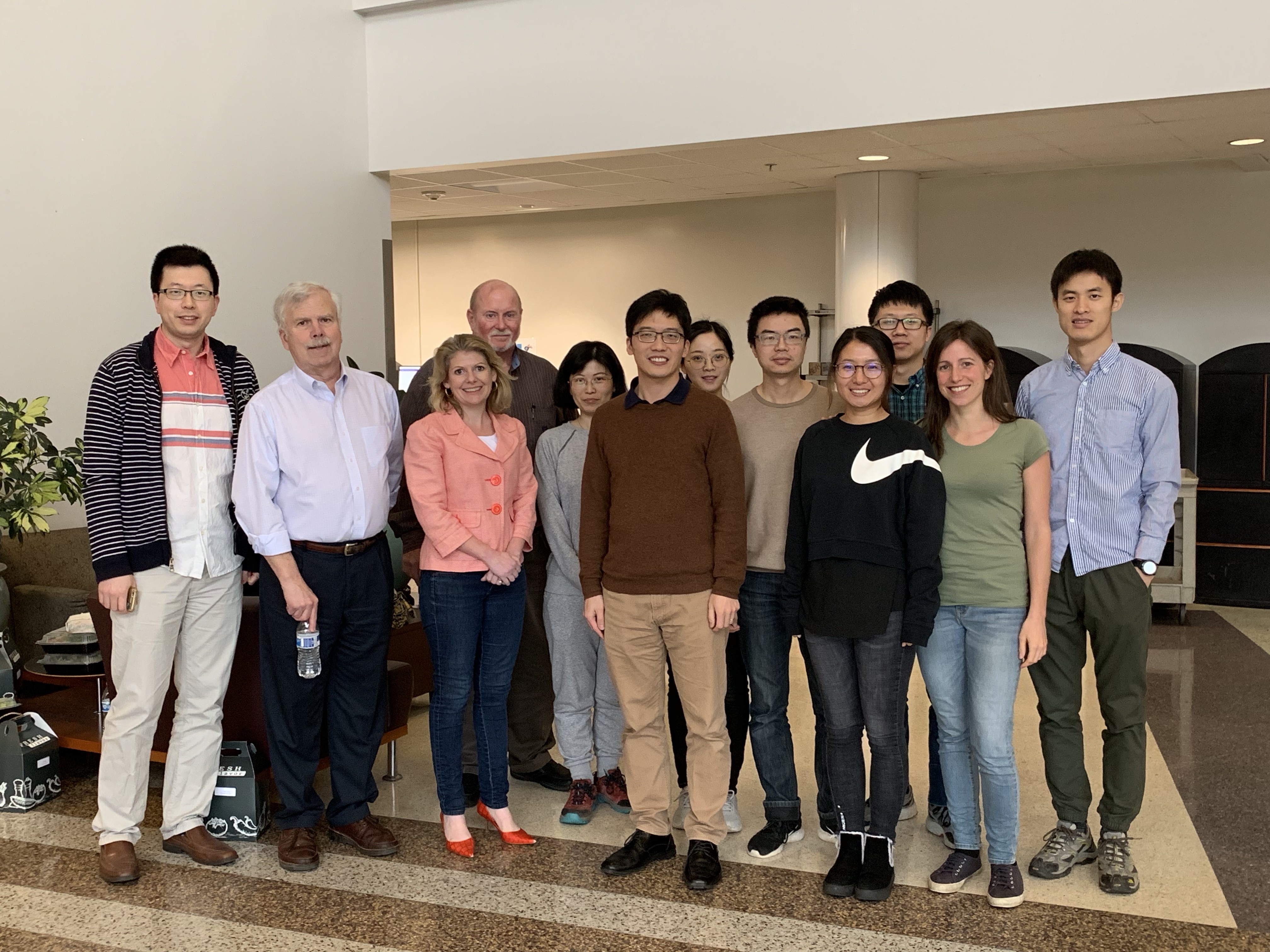
Qing Zhang Lab Team at UNC Lineberger Comprehensive Cancer Center
On March 1st, KCCure had the opportunity to tour the Qing Zhang Lab at UNC, meet the entire research team and talk directly with Dr. Zhang about his research in kidney cancer.
Your lab has a specific focus on hypoxic tumors that are resistant to standard therapy, including kidney cancer. What is hypoxia and why does it matter so much in kidney cancer tumors?
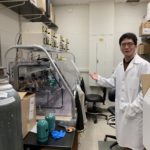
Dr. Zhang shows us lab equipment that allows them to mimic low oxygen environments to better understand tumor growth.
Hypoxia is a deficiency of oxygen. 85 percent of kidney cancer patients have a loss of the VHL tumor suppression gene. Loss of VHL leads to an increase in Hypoxia Inducible Factor (HIF).
Imagine that a tumor grows like a ball. When it gets bigger and bigger the center gets further away from blood vessels, which means a lack of oxygen, or hypoxia. When treated with chemo or radiation you would kill most of the oxygen-rich tumor on the periphery, but it is difficult to treat the center of the tumor that is oxygen-deprived. That hypoxia contributes to the radiation or chemo-resistant tumors in patients; and those leftover tumors in a hypoxic area could become malignant and metastasize in different organs. The fundamental question we’re trying to understand is how hypoxia signaling can contribute to tumor progression, and how we can design strategies to target this hypoxia signaling in cancer treatment.
Your latest research is focused on something called TBK1. What is TBK1?
When patients lose VHL, they will likely develop kidney cancer. When VHL is lost, our research found that one particular kinase, TBK1 showed increased activity. We wanted to look into that and see what it might mean for kidney cancer. Our research showed that getting rid of TBK1 slowed down kidney cancer cell growth.
How would this be used to fight kidney cancer in patients?
We think that TBK1 can be used as a good potential target for therapeutic intervention in kidney cancer. Unlike other targets used in kidney cancer, TBK1 is unique to kidney cancer cells that have VHL loss — so normal cells would be spared. That means, if successful, this therapy might have fewer side effects for patients.
We will also test the potential enhanced therapeutic efficacy by combinational targeting TBK1 and currently FDA approved kidney cancer therapies in kidney tumorigenesis. Our research will provide insight on validating TBK1 as a new therapeutic agent that would be beneficial for the majority of patients with kidney cancer.
We thank Dr. Zhang and his team for meeting with us. Without generous donors, we wouldn’t be able to fund exciting new research like Dr. Zhang and Dr. Tan’s work looking at TBK1 as a potential new therapy option in kidney cancer. Grants like KCCure’s Innovation Award help researchers learn more and build evidence to compete for larger awards that will move their research into clinical practice for patients. Learn more about Qing Zhang, his story and his research here!