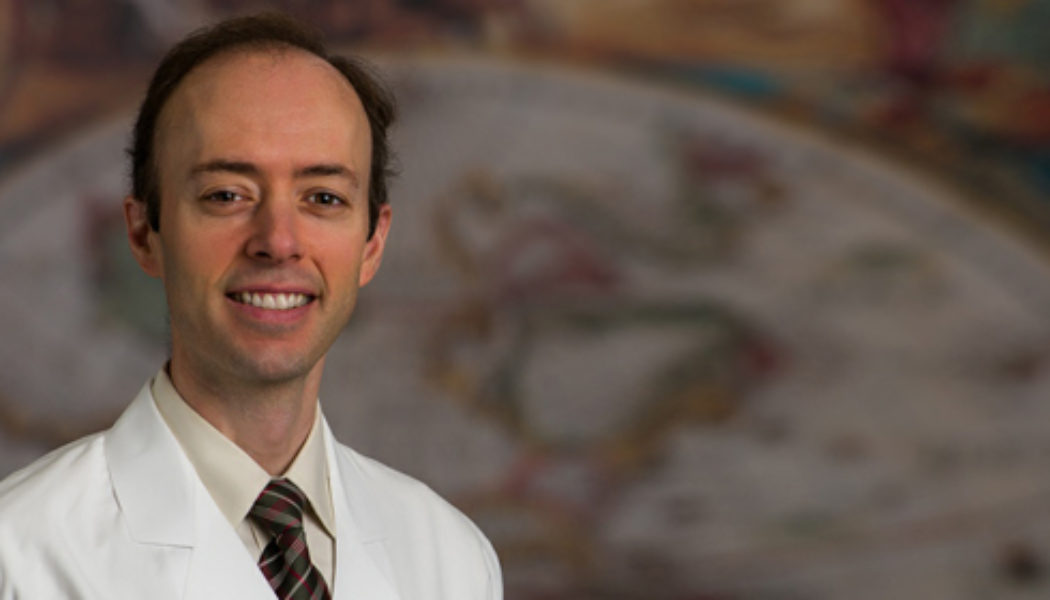
UT Southwestern Medical Center’s Harold C. Simmons Comprehensive Cancer Center has received the highly competitive Specialized Program of Research Excellence (SPORE) award from the National Cancer Institute (NCI). The grant will provide $11 million in funding. It is the first such award for kidney cancer research earned by a single institution, and only the second in the nation. To discuss the award, here is an interview with UTSW’s Principal Investigator Dr. James Brugarolas.
What types of projects do SPORE grants support?
SPORE grants involve both basic and clinical/applied science, and are intended to support projects that will result in new and diverse approaches to the prevention, early detection, diagnosis, and treatment of human cancers.
What are the areas that each SPORE focuses on?
Each SPORE focuses on a specific organ site, such as kidney or lung cancer, or on a group of highly related cancers either anatomically, such as gastrointestinal cancers, or biologically (deregulation of the same pathways).
How do SPOREs work, and what are they exactly designed to do?
SPOREs are designed to enable the rapid and efficient movement of basic scientific findings into clinical settings, as well as to determine the biological basis for observations made in individuals with cancer or in populations at risk for cancer.
Why is there a need for a SPORE grant in the area of kidney cancer research?
Kidney cancer is often detected after it has spread, at which point it is largely incurable. Thus, despite significant progress leading to the development of new therapies, new approaches are required. The rate of kidney cancer has been growing over the course of the last decade but why this is the case is unclear.
While there are about 50 SPORE grants across different cancer types in the country, there has been only one grant in kidney cancer. In fact, since the beginning of the SPORE program by the National Cancer Institute in 1992, there has been only one other SPORE grant in kidney cancer at the Dana-Farber/Harvard Cancer Center. The UTSW SPORE is the second SPORE grant for kidney cancer in the history of the SPORE program and the first grant to be awarded to a single institution.
What are some of the priorities in kidney cancer research that the funds from the SPORE grant will be used for?
Funds will be used to contribute to the development of a first-in-class drug targeting, arguably, the most important driver of kidney cancer, a protein called HIF-2. We hope to identify patients most likely to respond to this drug and characterize means of tumor escape. In addition, SPORE funding will be used to evaluate the impact on prognosis and therapy of molecular subtypes of adult and childhood kidney cancer we have discovered. Finally, we will utilize novel technologies to distinguish small tumors of low clinical significance from aggressive tumors that can become life-threatening. The SPORE will also support a much needed infrastructure involving a pathology core, an imaging core, and a data analytics core.
Can you provide some examples of discoveries made through kidney cancer research at UTSW that are paving the way for the development of the next generation of kidney cancer treatments?
UTSW scientists discovered what is regarded as the most important driver of adult kidney cancer (HIF-2) and identified a vulnerability in the protein structure that was exploited for drug development. That discovery led to the founding of a company in the UTSW BioCenter, Peloton Therapeutics, Inc, that developed a drug that is now in clinical trials at UTSW. Our work provided the first evidence that the HIF-2 blocking drug is active against kidney cancer using transplantation models (human kidney cancer into mice) and we have discovered candidate biomarkers that identify tumors most likely to respond.
UTSW has also made important discoveries in the molecular genetics of both adult and childhood kidney cancer. We discovered that the BAP1 gene is mutated in adult kidney cancer and that tumors with mutations in BAP1 tend to be particularly aggressive. Furthermore, we found that some familial kidney cancers result from mutations in BAP1 that are passed from parents to their children. UTSW pediatric oncologists also discovered that the DROSHA gene is mutated in childhood kidney cancer and that mutations in DROSHA, as well as in a second gene, DICER, identify a novel subtype of pediatric kidney cancer.
In addition, our surgeons have developed novel surgical approaches that require minimal incisions for kidney cancer surgery and our radiation oncologists have developed innovative approaches deploying stereotatic radiotherapy to treat life-threatening kidney cancer complications such as tumor thrombi that can sometimes invade all the way into the heart.
Technological innovation from the advanced imaging center to measure nutrient uptake and metabolism in tumors (in particular brain tumors) is also being deployed to evaluate kidney cancer.
What is your vision for advances in treatment of kidney cancer in the next 10 years?
We are making an investment in immunotherapy. UTSW has made seminal discoveries in immunology that we are translating into the clinic. Dr. Beutler discovered Toll-like Receptors (TLRs) and Dr. Chen the cGAS-STING pathway. These two pathways play critical roles in inflammation and the activation of the immune system. With recruits such as Dr. Hans Hammers we are looking for ways to translate these discoveries into new approaches to help patients.